
Lindsay, a 25-year-old data analyst, suffered with abdominal pain for years before being diagnosed with endometriosis. “My first symptom was pelvic pain. I'd had emergency surgery to remove a large ovarian cyst, and thought that the pain I was experiencing was related to that, but it didn't subside after the cyst was taken care of.” Lindsay is not alone in suffering from endometriosis. It affects 1 in 10 women worldwide and there are currently no guidelines to prevent it.
Normally, endometrial tissue is found only inside the uterus. The uterus is the reproductive organ where a fetus develops. Hormones cause the tissue to form there, preparing the body for a fertilized egg. If you do not become pregnant, the tissue leaves the body during menstruation.
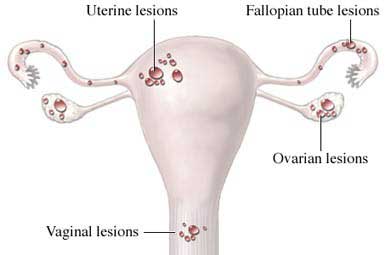
In endometriosis, endometrial-like tissue is found outside the uterus. Typically it is found in the pelvic cavity but, occasionally, endometriosis may be found in the bladder, bowel, intestines, appendix or rectum. In these places, the tissue still responds to hormones. It swells, breaks down, and bleeds, but it is unable to leave when you menstruate. Surrounding tissue becomes inflamed and there is often scarring.
Endometriosis
Copyright© Nucleus Medical Media, Inc.
What Causes Endometriosis?
Possible causes include:
- Menstrual tissue backs up through the fallopian tubes and spills into the abdomen.
- Immune system may allow the tissue to implant on other organ surfaces and develop into endometriosis.
- Lymph system may carry endometrial cells from the uterus.
- Certain cells left behind on abdominal organs during embryonic development can turn into endometrial tissue.
Hormones and growth factors cause the disease to progress.
Risk Factors
Endometriosis often begins in the teen years and develops slowly over the course of a woman’s life. Its causes are not fully understood, and genetic factors are believed to play a primary role in its occurrence.
Factors that may increase your risk of endometriosis include:
- Family history—a mother or sister with endometriosis.
- Early onset of menstruation.
- Not having children—Pregnancy slows or stops the disease from progressing. The condition usually resolves at menopause. The symptoms may return with hormone replacement therapy.
- Prolonged menstrual bleeding—more than 7-8 days.
- Abnormal development of the uterus, with a blocked segment.
Symptoms
Symptoms of endometriosis range from mild to severe. You may have many large growths with little pain. Or, you may have small areas with intense pain. Symptoms include:
- Cramping and pelvic pain—especially just before and during menstrual bleeding.
- Pain during sex— dyspareunia.
- Heavy periods.
- Low back pain.
- Pain during bowel movements or urination.
- Infertility.
- Miscarriage.
Diagnosis and Treatment
You will be asked about your symptoms and medical history, and a pelvic exam will be done. These are best done early in the menstrual period. Since you may not have any symptoms, diagnosis is usually confirmed with a laparoscopy, a test that allows the doctor to see if there are patches of endometrial tissue and scar tissue.
Once diagnosed, the goals of treating endometriosis are to:
- Control pain.
- Slow endometrial growth.
- Restore or preserve fertility.
Treatment options depend on:
- Severity of symptoms.
- Size, number, and location of growths.
- Degree of scarring.
- Extent of the disease.
- Age and whether you want to have a baby.
Treatment options include:
Pain Medication
Your doctor may recommend:
- Over-the-counter pain relievers to ease mild symptoms.
- Nonsteroidal anti-inflammatory drugs to reduce inflammation and help with cramping—best taken on a regular basis.
Hormonal Therapy
Hormones are an option for women who are not trying to become pregnant. Birth control pills and other injectable drugs interfere with estrogen production. These medications may decrease pain and shrink the size and number of endometrial growths. Symptoms and endometrial growths tend to come back when the hormones are stopped, though. If birth control pills are prescribed to manage endometriosis, then they often are used continuously, so that you do not menstruate. After surgery, birth control pills may reduce the chance of endometrial growths returning.
Surgery
If you have severe symptoms or you want to get pregnant, doctors can try to remove endometrial growths. This is often done with laparoscopic surgery. In severe, unmanageable cases it may be advised to also remove the uterus and ovaries, but this means that you cannot get pregnant.
In Conclusion
After treatment Lindsay is recovering and has this advice for other women. “Keep a pain journal. I've found this to be very important both in managing my own illness—I was able to see, for instance, a link between my caffeine consumption and pain—and in helping doctors to see patterns that can guide treatment. People, doctors, and friends alike also take you more seriously when you're able to demonstrate exactly what you're experiencing and when you felt it. I made a chart based on a 28-day cycle and kept track of things I ate or drank that might be potential triggers, when I had discomfort, and what seemed to make me feel better. I also sought out the support of other women with endometriosis. No one can really understand until they've been through it themselves.”