A lifechanging treatment option for essential tremor, Parkinson’s disease, and dystonia
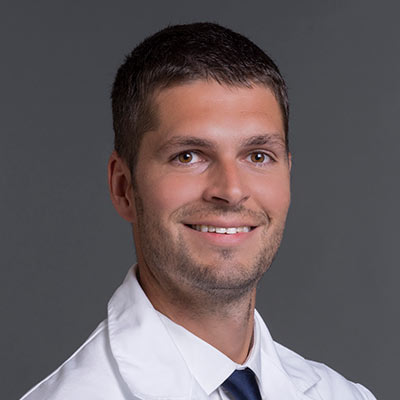
Gareth Davies, MD, is a board-certified and fellowship-trained neurosurgeon with Coastal New Hampshire Neurosurgeons in Portsmouth, New Hampshire, and is affiliated with Portsmouth Regional Hospital, the Seacoast Region’s leader in neurological care. He provides advanced surgical care for a wide range of neurological conditions, with specialized expertise in deep brain stimulation (DBS) to treat movement disorders that affect the brain and spine.
What is DBS?
DBS is a lifechanging surgical treatment option for patients with diagnosed movement disorders that have not responded to traditional medications. The goal of DBS is to maximize quality of life and range of motion by improving communication between the neurons in the brain. The result is a vast reduction in the stiffness and involuntary tremors often associated with these disorders. During the DBS procedure, electrodes are placed deep within the brain to generate mild impulses that help regulate electrical activity, much like a pacemaker in the heart normalizes its rhythm.
Movement conditions most commonly considered for DBS include:
- Essential tremor
- Parkinson's disease
- Dystonia
Researchers are investigating if DBS also could be considered as a treatment option for other types of conditions that may be resistant to traditional medication, including:
- Tourette syndrome
- Obsessive-compulsive disorder
- Chronic pain
- Dementia
- Depression
- Addiction
- Severe Headaches
- Huntington's disease
What happens during DBS surgery?
Prior to the DBS procedure, detailed scans of the brain using magnetic resonance imaging (MRI) and computed tomography (CT) are taken to help determine optimal placement of electrodes. The DBS operation usually takes place as a two-part procedure—the first operation is to place the electrodes within the brain, and the second operation is to implant a pulse generator device in the upper chest and connect it to the electrodes.
During the first procedure, which usually takes between four and six hours, the patient is sedated and a special frame is attached to the head to prevent movement. The neurosurgeon makes an incision in the scalp and a small hole in the skull, roughly the size of a dime. Patients may feel some vibrations and hear the surgical drill but will not experience pain. A specialized delivery system precisely positions the electrodes into the area of the brain that controls bodily movements. The majority of patients experience an immediate, marked reduction in their disease symptoms while still in the operating room.
One to two insulated wires, also called leads, are connected to these electrodes. The leads are then threaded around the brain and under the skin of the neck. Throughout the remaining surgery, patients remain mildly sedated but are awake and interactive with the surgical team to help determine optimal positioning of the electrodes within the brain. The goal is to have the greatest impact on reducing any tremors, rigidity, or dyskinesia, with the least number of side effects. Patients typically spend only one night in the hospital and return about a week later for the pacemaker device to be implanted.
During the second procedure, done under general anesthesia, a small pulse generator pacemaker device is implanted under the skin near the upper chest. The leads that are connected to the electrodes within the brain are attached to the pacemaker, which is uniquely programmed for each patient to optimize signals to the brain. This is an outpatient procedure, so patients are able to go home the same day but will have some activities restricted for several weeks.
In the days following surgery, the neurosurgical team will adjust the amplitude of the pacemaker device to maximize the benefits to the patient, while minimizing any side effects. The device has a built-in, wireless antenna, so it also can be programmed and adjusted by the surgical team while the patient is at home. In addition, patients are given a remote control to turn their pacemaker device on or of, and sometimes to make minor adjustments to the amount of stimulation.
Who are good candidates for DBS?
Patients diagnosed with essential tremor, Parkinson’s disease, and dystonia, who are otherwise in good health, make good candidates for DBS. They must be able to actively engage with the surgical team during the procedure, so patients experiencing dementia are not viable candidates.
Ultimately, it is the decision of the patient if medication is no longer enough to manage their condition and they are ready to consider DBS.
What are the advantages of DBS and what impact does it have on a patient’s life?
While not a cure for conditions like essential tremor and Parkinson’s disease, DBS often has a lifechanging impact on managing the debilitating symptoms of these disorders. Many patients see immediate improvement in their severe tremors, allowing them to resume normal daily activities like eating, drinking, and writing that many individuals had no longer been able to do on their own.
Are there potential risks and side effects related to DBS?
All surgeries come with some risk, but, in general, DBS is regarded as a minimally invasive, low-risk procedure. The goal is to place the leads where the patient ideally experiences no side effects. Since the patient communicates with the surgical team throughout the DBS procedure, side effects are minimized or eliminated.
When the pacemaker stimulation device is turned off, the patient does not experience side effects. When on, potential side effects depend upon where the leads were implanted in the brain and may include:
- Flashing lights or double vision
- Difficulty with speech
- Numbness or tingling
- Difficulty with balance
The neurosurgical team will program the pacemaker device so that the patient is able to toggle between options to reduce any side effects. While DBS is highly successful, it is reversible if the patient is not able to tolerate potential side effects.
Why choose Coastal New Hampshire Neurosurgeons and Portsmouth Regional Hospital?
Portsmouth Regional Hospital is only one of two hospitals in all of New Hampshire offering DBS. Dr. Davies is board-certified and fellowship-trained in neurosurgery with specialized expertise in DBS. He is the only neurosurgeon offering DBS in Portsmouth and surrounding Seacoast Region, offering patients and their loved ones convenient access to an expert neurosurgeon. Since the procedure is performed in two parts and requires follow up visits, there are advantages to choosing DBS close to home.
To learn more or to schedule a consultation with Dr. Davies, call (603) 433-4666 or book an appointment online.